While it was like only yesterday that people were calculating the day they could feel fully protected by their vaccination, now scientists are saying our safety may require another shot in the arm.
This booster conversation is gaining urgency as the Delta variant causes a surge among both vaccinated and unvaccinated individuals and health officials, with its centre place being Africa. Scientists in the last months have clearly shared that the available vaccines might not fully protect against the virus.
The Food and Drug Administration (FDA) has now recommended a third dose of Pfizer or Moderna vaccines to increase immunity against Covid-19. The FDA recently amended the emergency use authorizations (EUA) for Pfizer-BioNTech and Moderna to allow an additional dose of their COVID-19 vaccines for certain immuno-compromised people. The list includes solid organ transplant recipients and those with conditions that give them an equally reduced ability to fight infections and other diseases.
What is a booster?
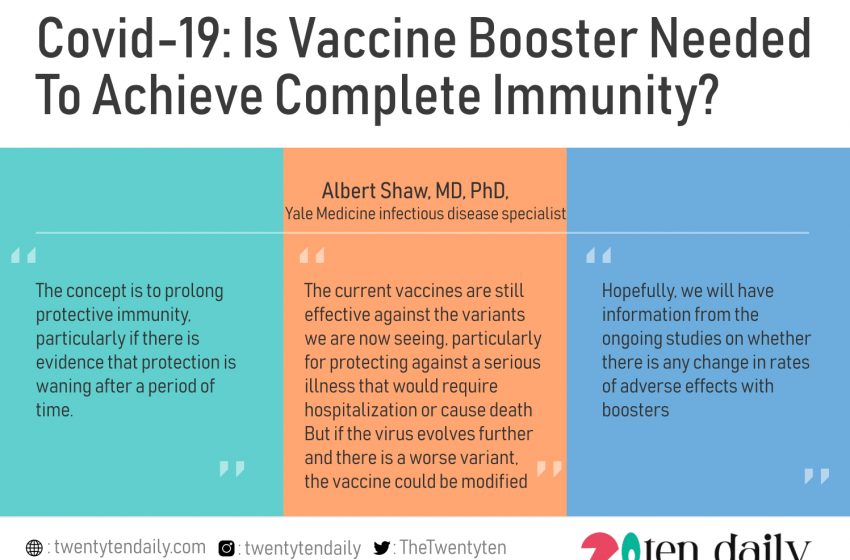
“The simplest answer is that it’s just another dose of a vaccine you received,” according to Albert Shaw, MD, PhD, a Yale Medicine infectious disease specialist. “The concept is to prolong protective immunity, particularly if there is evidence that protection is waning after a period of time.”
Most children receive routine vaccinations, including boosters, for illnesses such as chickenpox, tetanus, diphtheria, mumps, measles, and rubella—to name a few. “These vaccine series, as we call them, are recommended because you need the extra doses to get longer-lasting protective immunity,” Dr Shaw explains.
Why might we need a booster for COVID-19?
While a booster sometimes is an exact replica of the initial vaccine, it can also be tweaked. With COVID-19, this is key because the vaccine could then be tailored to target particular variants of the virus.
“The current vaccines are still effective against the variants we are now seeing, particularly for protecting against a serious illness that would require hospitalization or cause death. But if the virus evolves further and there is a worse variant, the vaccine could be modified,” Dr Shaw says.
One of the great things about the mRNA technology, which the Pfizer and Moderna vaccines use, Dr Shaw notes, is that it’s easy to change them up to match variants, and they can be quickly produced at scale. “This is different from the manufacturing process for the most commonly used flu vaccines, which is a much slower process because influenza virus strains need to be grown in chicken eggs, from which a particular viral protein is purified and formulated into a vaccine,” he says.
Should a booster shot only be for certain people?
When COVID-19 vaccines first became available, they were first offered to the most vulnerable, including older adults. People who are immunocompromised have also been given priority, which may explain why the FDA recently approved a third dose of Pfizer’s and Moderna’s vaccines in that population.
Could you mix and match vaccines in a booster?
So-called “mixing and matching” of vaccines (the first dose of Pfizer, followed by a second dose of Moderna, for example, to complete the mRNA two-dose series) has been used in Europe and other places, particularly when there were supply issues. And there have been recent studies suggesting this approach—with one dose of AstraZeneca’s vaccine (which is not available in the U.S.) and one dose of Pfizer’s vaccine—may even offer more vigorous protection. But here in the U.S., the current public health recommendations are that people should stick with one type of mRNA vaccine for both doses.
But what about boosters—if they are recommended, should you stick with your original kind?
“That is being evaluated right now. The NIH [National Institutes of Health] is sponsoring a study that is ongoing and hopefully, we will have answers to that,” Dr Shaw says.
Could a booster cause more or worse side effects?
If you were among the unlucky recipients who felt really ill or had any of the rare but largely harmless reactions to your initial COVID-19 vaccination, you may be leery of the idea of a third dose, in case it causes a similar or worse reaction.
“Hopefully, we will have information from the ongoing studies on whether there is any change in rates of adverse effects with boosters,” Dr Shaw says. “It’s reassuring that for the vast majority of individuals, the currently used vaccines have been safe, and if I had to guess, I would say rates of any problems would remain very low.”
In the main time, specialists still emphasize that the most important thing any of us can do is get vaccinated. And if you are already vaccinated, know that the situation is being closely monitored by the scientific and public health communities.