While the world focuses on the novel coronavirus, new reports are cautioning on a potential outbreak of another virus called the Nipah Virus.
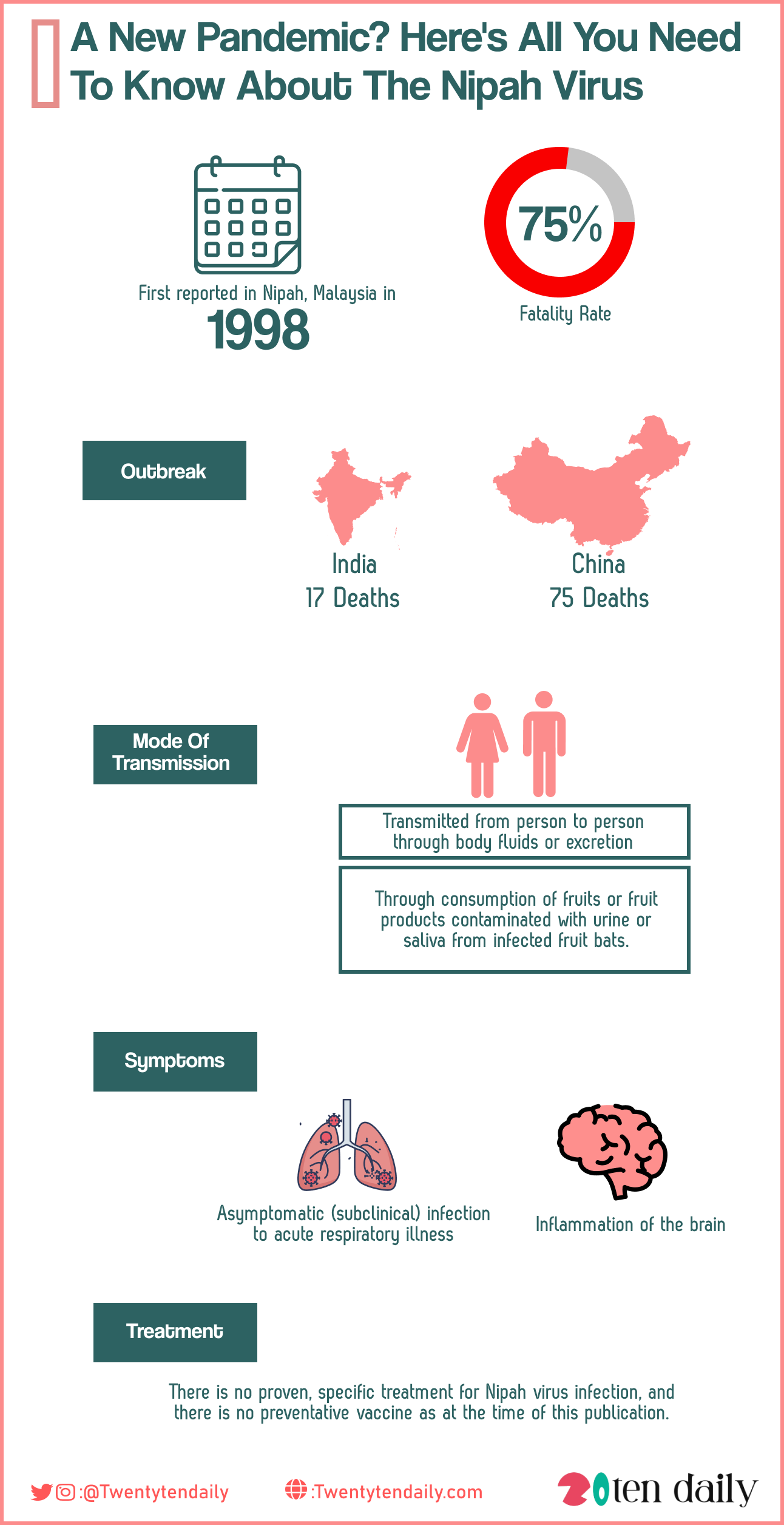
First reported in Nipah, Malaysia in 1998, outbreaks have subsequently occurred in parts of North East India, Singapore, Philippines and most recently China. The Nipah virus outbreak in China had a fatality rate of up to 75 percent hence the reason experts believe it might potentially be the next big pandemic risk.
Epidemiology
The virus is transmitted from animals to humans, it is found in contaminated food. It can also be transmitted from person to person through body fluids or excretion. During the first recognized outbreak in Malaysia, most human infections resulted from direct contact with sick pigs, or their contaminated tissues.
Later outbreaks in Bangladesh and India was through consumption of fruits or fruit products (such as raw date palm juice) contaminated with urine or saliva from infected fruit bats.
Human-to-human transmission of Nipah virus has also been reported among family and caregivers of infected patients. Risk of infection in other regions is possible, as evidence of the virus was found in the known natural reservoir (Pteropus bat species) and several other bat species in some countries, including Cambodia, Ghana, Indonesia, Madagascar, the Philippines, and Thailand.
During the later outbreaks in Bangladesh and India, Nipah virus spread directly from human-to-human through close contact with people’s secretions and excretions. In Siliguri, India in 2001, the transmission of the virus was also reported within a health-care setting, where 75 percent of cases occurred among hospital staff or visitors. From 2001 to 2008, around half of the reported cases in Bangladesh were due to human-to-human transmission by providing care to infected patients.
An outbreak of the Nipah virus in India’s southern state Kerala in 2018 claimed 17 lives and a later outbreak in China claimed 75 lives.
Symptoms Of Nipah Virus
According to the World Health Organization (WHO), the virus can cause a range of illnesses from asymptomatic (subclinical) infection to acute respiratory illness or fatal causes of encephalitis, or inflammation of the brain.
Symptoms typically surface 4-14 days after exposure to the virus. The patient experiences 3-14 days of fever and headache and often includes signs of respiratory illness, such as cough, sore throat, and difficulty breathing. A phase of brain swelling (encephalitis) may follow, where symptoms can include drowsiness, disorientation, and mental confusion, which can rapidly progress to coma within 24-48 hours.
Death may occur in 40-75% of cases. Long-term side effects in survivors of Nipah virus infection have been found that includes persistent convulsions and personality changes.
Treatment
There is no proven, specific treatment for Nipah virus infection, and there is no preventative vaccine as at the time of this publication.
Patients have been reportedly treated with Ribavirin in previous outbreaks, but it was not possible to determine the beneficial effect of treatment. Ribavirin was ineffective in small animal models, as was chloroquine. Several experimental therapies are in pre-clinical development or phase 1 clinical trials, including monoclonal antibodies, fusion inhibitors, and novel antivirals.
Nipah virus is one of the pathogens in the WHO R&D Blueprint list of epidemic threats requiring urgent research and development action, including animal and human vaccine development. Further information on experimental therapies and vaccine development is available from WHO.
Travel Caution for travellers to endemic areas
Those travelling to endemic areas, particularly areas with active outbreaks, should avoid contact with bats and their environments, and sick animals. Consumption of raw or partially fermented date palm sap should be avoided. Wash fruits with clean water and avoid any fruit that has been partially eaten by animals or that may be contaminated.
Travellers are also advised to practice social distancing and to wear nose masks at public gatherings or outings. For further information about the virus, see WHO Nipah virus collection.

